 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
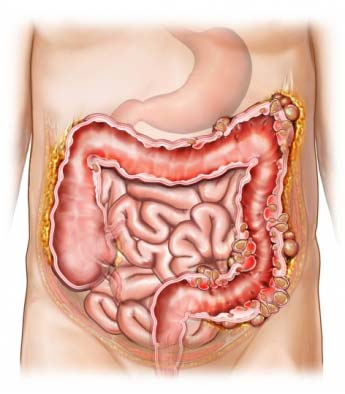
The Digestive System
Sometimes referred to as the gastrointestinal (GI) tract, is made up of several important digestive organs, such as:
“It is very simple to wrongly ignore gastrointestinal symptoms problems because there are so many distinct kinds of them. Although some GI issues are minor and often go away on their own, some issues are severe enough that you need to visit a doctor or gastroenterologist”.
For women under 50, consuming 25 grams of fiber daily is advised, while males under 50 should consume 38 grams. You should eat a little less if you are over 50. (around 21 grams for women and 30 grams for men). The good news is that foods like fruits (nearly totally in the skin, though), whole grains, lentils, beans, and vegetables are rich sources of fiber. A diet low in fiber can be a fantastic method to assist with constipation, stomach pain, and even the start of colon cancer. It can also help with bloating and improve digestive issues.
- The Mouth
- Esophagus, sometimes known as the "feeding pipe"
- Stomach
- The big and small bowels
- Anus, and the rectum
An expert says
The Typical Symptoms of Digestive Issues
Clearly, each individual's and condition's signs and symptoms for gastrointestinal disease are unique. However, the majority of digestive problems exhibit certain indications and symptoms. Common symptoms include:- Discomfort in the stomach (bloating, pain or cramps)
- Inadvertent weight loss • Nausea and vomiting • Acid reflux (heartburn)
- Diarrhea and indigestion (or sometimes both)
- Difficulty swallowing; • Fatigue; • Loss of appetite; • Fecal incontinence
“Remember, a medical professional's thorough diagnosis and treatments are the only ways to address these issues and eliminate these symptoms”, advises specialist.
What causes stomach problems?
Consistent gastrointestinal issues include:A Diet Low in Fiber
When it comes to digestive health, fiber, a kind of carbohydrate abundant in plants but not digestible, is essential. It promotes satiety and assists in the digestion of some meals. Everyone is talking about the importance of fiber for gut health and the health of your microbiome. Fibers help the billions of beneficial bacteria (your microbiota) that happily live in our big intestine, which has a variety of great health impacts.For women under 50, consuming 25 grams of fiber daily is advised, while males under 50 should consume 38 grams. You should eat a little less if you are over 50. (around 21 grams for women and 30 grams for men). The good news is that foods like fruits (nearly totally in the skin, though), whole grains, lentils, beans, and vegetables are rich sources of fiber. A diet low in fiber can be a fantastic method to assist with constipation, stomach pain, and even the start of colon cancer. It can also help with bloating and improve digestive issues.
Being Stressed
In addition to their detrimental impact on your mental health, stress and anxiety can also affect your digestive health, especially the gut flora. Recent medical research have revealed a connection between the GI system and the brain. The stomach contains more neurons than the entire spinal cord because the two are always in touch with one another and delivering messages to one another. A wide range of digestive problems, such as appetite loss, inflammation, bloating, cramps, and changes in microbiota, have been linked to stress. inflammation, bloating, cramps, and changes in microbiota,
"These are only a few typical reasons why people develop digestive issues. According to Dr. Guandalini, additional factors may include lifestyle choices, drug interactions, pregnancy, excessive laxative use, functional problems, inflammation, and systemic illnesses.
Inadequate Water Consumption
Since it helps to cleanse the gastrointestinal system, water is essential for digestive health. Particularly water aids in preventing constipation by softening the stool. More significantly, water is thought to benefit your digestive system by facilitating food digestion, which allows the GI tract to absorb nutrients more rapidly and effectively. A variety of gastrointestinal problems might result from a lack of water consumption. To meet your daily target of 8 glasses of fluids, you can increase your water intake by drinking unsweetened coffee, tea, or even sparkling water! Just steer clear of sugary drinks like soda!Consumption Of Dairy-Based Foods
Dairy is a very recent addition to the human diet; throughout the first 200,000 years or so of human history, it was not really consumed. Milk and cheeses are frequently packed with indigestible lipids and proteins that, per some medical research, have an inflammatory impact. Because of this, ingesting a lot of dairy products might result in bloating, gas, constipation, and cramping in the abdomen.Inactive Way Of Life
Your digestive system's health as well as your general health will suffer if you don't exercise enough. To treat specific GI issues, doctors often advise a mix of exercise, diet adjustments that limit intake of items that aggravate inflammation while boosting intake of nutrients that actually reduce it.Aging
Unfortunately, as people age, their propensity for gastrointestinal diseases increases. Digestive gland activity declines with aging, which has an impact on gut motility, reflux, and the emergence of certain digestive diseases. With advancing age, so is the danger of getting malignancies of the digestive system.Genetic Effects
Your genes are yet another inescapable factor! Numerous gastrointestinal immunological and autoimmune illnesses have a genetic foundation, making them inherited conditions. Sometimes, only these altered genes are required for the development of a Gi disease (think cystic fibrosis, or hereditary pancreatitis). Fortunately, most of the time they only predispose you to the disease, indicating that environmental variables must also be at play. This indicates that, even while your genes play a role in the tale, they don't hold the whole picture. Alterations to one's way of life can assist. Ulcerative colitis, Crohn's disease, celiac disease, and a few liver diseases are a few examples of hereditary illnesses that are predisposed."These are only a few typical reasons why people develop digestive issues. According to Dr. Guandalini, additional factors may include lifestyle choices, drug interactions, pregnancy, excessive laxative use, functional problems, inflammation, and systemic illnesses.
The top 13 digestive diseases include:
The small intestine cannot efficiently absorb nutrients, vitamins, and minerals from meals when the villi are damaged. Malnutrition as a result can cause a host of major health issues, such as infertility, small intestine damage that cannot be reversed, and even the deadly intestinal lymphoma, or the big "C." For this reason, celiac disease and having a correct diagnosis are crucial.
Around 1% of people worldwide (including those in the US) are thought to have celiac disease. Thus, one American out of every 100 has celiac disease. Previously believed to be uncommon, celiac disease is today one of the most prevalent autoimmune illnesses.
Children and adults with celiac disease may have both digestive and extraintestinal symptoms. These symptoms, which include headaches, tiredness, joint discomfort, anemia, skin rashes, hair loss, irregular menstruation, miscarriage, infertility, weak bones, tooth discolouration, and even convulsions, are not related to the intestines. As you can see, celiac disease manifests itself in a variety of ways!
A precise diagnosis is necessary. Never "attempt" to cut gluten out of your diet without first getting tested for celiac disease! The avoidance of gluten has dangers. A preliminary blood test is part of the testing process, and if it indicates a potential case of celiac disease, a small intestinal biopsy is next. Be at ease; the treatment is short, safe, and painless and is carried out by pediatric or adult gastroenterologists. Remember that in order for the findings of the biopsy and blood test to be precise, you must still consume gluten.
Contrary to popular belief, this ailment is not the same as Inflammatory Bowel Disease (IBD), a group of digestive disorders that include Crohn's disease and ulcerative colitis that cause inflammation of different areas of the gastrointestinal system. 3 to 20 percent of Americans suffer from irritable bowel syndrome. Stress and the use of particular medications and meals are a few risk factors. IBS is more common in women than in males.
However, a variety of conditions, such as celiac disease, food allergies and intolerances, Crohn's disease and ulcerative colitis, IBS, and ulcerative colitis can result in persistent diarrhea. These conditions must be properly diagnosed in order to receive the appropriate therapy. Numerous intestinal infections, including Giardia, C. difficile, and Cryptosporidium, can also cause chronic diarrhea.
- Celiac Disease
- Irritable Bowel Syndrome (IBS)
- Lactose Intolerance
- Chronic Diarrhea
- Constipation
- Gastroesophageal Reflux Disease (GERD)
- Peptic Ulcer Disease
- Crohn’s Disease
- Ulcerative Colitis
- Gallstones
- Acute and Chronic Pancreatitis
- Liver Disease
- Diverticulitis
Celiac disease
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
A multifactorial digestive ailment, celiac disease. That's a fancy way of explaining that although it has hereditary roots, environmental variables contribute to its onset. An immunological response to the protein gluten, which is present in grains including wheat, rye, barley, and their hybrids, is what causes celiac disease. Gluten causes an immune response in a person with celiac disease that kills the villi, which are tiny hair-like projections on the lining of the small intestine.
The small intestine cannot efficiently absorb nutrients, vitamins, and minerals from meals when the villi are damaged. Malnutrition as a result can cause a host of major health issues, such as infertility, small intestine damage that cannot be reversed, and even the deadly intestinal lymphoma, or the big "C." For this reason, celiac disease and having a correct diagnosis are crucial.
Around 1% of people worldwide (including those in the US) are thought to have celiac disease. Thus, one American out of every 100 has celiac disease. Previously believed to be uncommon, celiac disease is today one of the most prevalent autoimmune illnesses.
Symptoms:
The digestive system is impacted by celiac disease symptoms, but they can also appear elsewhere on the body. Some folks might not even exhibit any symptoms. However, it's important to remember that symptoms vary often between adults and children. Children with celiac disease, for instance, may have shorter statures, delayed puberty, and a propensity for moodiness and exhaustion. Children and adults with celiac disease might have the same digestive symptoms, including foul-smelling stools, diarrhea or constipation, stomach discomfort, abdominal bloating, vomiting, and weight loss.Children and adults with celiac disease may have both digestive and extraintestinal symptoms. These symptoms, which include headaches, tiredness, joint discomfort, anemia, skin rashes, hair loss, irregular menstruation, miscarriage, infertility, weak bones, tooth discolouration, and even convulsions, are not related to the intestines. As you can see, celiac disease manifests itself in a variety of ways!
Treatment:
The cure for celiac disease is unknown. The good news is that these symptoms may generally be reduced and frequently stopped by strictly adhering to a gluten-free diet. Supplementing with multivitamins may support this permanent gluten-free diet.A precise diagnosis is necessary. Never "attempt" to cut gluten out of your diet without first getting tested for celiac disease! The avoidance of gluten has dangers. A preliminary blood test is part of the testing process, and if it indicates a potential case of celiac disease, a small intestinal biopsy is next. Be at ease; the treatment is short, safe, and painless and is carried out by pediatric or adult gastroenterologists. Remember that in order for the findings of the biopsy and blood test to be precise, you must still consume gluten.
Irritable bowel syndrome (IBS)
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Irritable colon, mucous colitis, nervous stomach, and spastic colon are other names for irritable bowel syndrome (IBS). IBS is a category of gastrointestinal disorders in which a person frequently feels bloated, crampy, and uncomfortable with either diarrhea or constipation. By definition, this happens in the absence of any underlying inflammation, chemical imbalances, or anatomical abnormalities. It can be brought on by a number of things, including a disturbed gut flora.
Contrary to popular belief, this ailment is not the same as Inflammatory Bowel Disease (IBD), a group of digestive disorders that include Crohn's disease and ulcerative colitis that cause inflammation of different areas of the gastrointestinal system. 3 to 20 percent of Americans suffer from irritable bowel syndrome. Stress and the use of particular medications and meals are a few risk factors. IBS is more common in women than in males.
Symptoms:
The duration and frequency of irritable bowel syndrome symptoms varies from person to person, and they can also affect teens and, less commonly, young children. While some people only have minor symptoms, others deal with severe symptoms that can impair their quality of life. Do not forget the importance of a correct diagnosis handled by gastroenterologists. Before presuming it is IBS, you need to be sure Crohn's disease, celiac disease, food allergies, and food intolerances have been properly ruled out.Treatment:
Depending on the kind of IBS (IBS-C with constipation, IBS-D with diarrhea, or IBS-Mixed, which alternates between diarrhea and constipation), treatment options for IBS may include:- Consuming more (or less!) fiber in your diet
- Reducing stress or finding coping mechanisms for it
- Getting rid of FODMAPs from your diet. FODMAPs, which are carbohydrates that are poorly absorbed in the small intestine, prone to absorbing water, and ferment in the colon where they cause discomfort, are found in large quantities in many plants. The best way to follow a low-FODMAP diet is with a dietitian or nutritionist's advice.
- Using probiotics to treat IBS
Intolerance to Lactose
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
An individual with lactose intolerance is unable to adequately digest lactose, a simple carbohydrate found in milk and its derivatives from all mammalian species. Low amounts of the lactase enzyme, which breaks down lactose, are to blame for this. Approximately 79% of Native Americans, 75% of African Americans, 51% of Hispanics, and 21% of Caucasians suffer with lactose intolerance, which is a highly prevalent ailment.
Symptoms:
Symptoms after consuming dairy products might be minor to upsetting. Gas, bloating, diarrhea, and stomach cramps are all signs of lactose intolerance. Due to varying degrees of intestinal lactase depletion, symptoms vary from person to person and generally depend on the quantity of lactose consumed.Treatment:
Treatments for lactose intolerance include taking enzyme supplements to aid in lactose digestion and switching to lactose-free or dairy-free milk in place of ordinary milk. As part of your diagnosis and therapy, it's crucial to distinguish between lactose intolerance, milk allergy, and dairy sensitivity.Chronic Diarrhea
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
A person with chronic diarrhea has bowel movements that are watery, mushy, or loose for more than four weeks. In a 2018 study, researchers discovered that 6.6 percent of Americans had chronic diarrhea. According to this, 6 to 7 Americans out of every 100 have the illness. This syndrome appears to be favored by a high daily sugar intake, being overweight, experiencing depression, being older, and being a woman.
However, a variety of conditions, such as celiac disease, food allergies and intolerances, Crohn's disease and ulcerative colitis, IBS, and ulcerative colitis can result in persistent diarrhea. These conditions must be properly diagnosed in order to receive the appropriate therapy. Numerous intestinal infections, including Giardia, C. difficile, and Cryptosporidium, can also cause chronic diarrhea.
Treatment:
Based on the underlying cause of your doctor's choice of the best course of action for treating your diarrhea. Steroids, antibiotics, pain relievers, immune suppressants, antidiarrheal drugs, and other prescription drugs may be included. Changes to one's diet and way of life may also help lessen the effects of persistent diarrhea.Indigestion
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Constipation is a digestive ailment in which bowel motions are less often than usual and are hard, dry, and usually uncomfortable (generally fewer than three bowel movements a week). Constipation, which is one of the most prevalent signs of digestive disorders, is thought to afflict about 2.5 million Americans.
Constipation may occasionally be brought on by anatomical or inflammatory disorders, but it is usually brought on by a low-fiber diet, insufficient or no exercise, dehydration, certain medications, such as sedatives and some antidepressants, or anything that alters your regular diet or routine.
All of this causes the feces to move more slowly through the colon, causing them to become harder and bigger while they sit in the rectum. Constipation is when you propensity to stretch during ejaculating, which can occasionally result in hemorrhoids and anal fissures.
Treatment:
Constipation is frequently managed by:- Increased consumption of fiber and water
- Consistent exercise (every day of the week is ideal)
- Paying attention to bowel movement impulses
Gastroesophageal Reflux Disease (GERD)
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Gastroesophageal reflux disease (GERD) is characterized as acid reflux symptoms occurring twice or more per week. Acid reflux, often known as heartburn, happens when stomach contents and acids leak into your esophagus, generating a burning feeling and chest discomfort. This disorder is also known as acid regurgitation. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Gastroesophageal Reflux Disease affects around 20% of Americans .
Frequent attacks of heartburn, if not addressed promptly, can cause esophagitis, esophageal constriction, and other major health consequences, including Barrett's esophagus, a precancerous lesion. Dry cough, chest pain, sore throat, swallowing difficulty, and other symptoms of GERD are common.
Treatment:
You may cure GERD by doing the following:- Changes in lifestyle: minimize weight, avoid acid-stimulating meals (caffeine, alcohol, fried, fat foods, tomato sauce), and go to bed at least 2 hours after eating anything.
- Taking antacids over-the-counter to relieve heartburn
- Using H2 receptor blockers (e.g., Famotidine) or proton pump inhibitors (such as Omeprazole and others)
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Peptic Ulcer Disease
Peptic Ulcer Disease (PUD) is a gastrointestinal disorder caused most usually by an infection with the bacterium Helicobacter pylori, in which ulcers or open sores develop in the stomach and duodenum lining (the first portion of the small intestine). A thick mucus layer generally protects the stomach lining from erosion by digestive fluids. When this protective barrier is compromised, peptic ulcers can develop. Aside from H.pylori, various other conditions, such as alcoholism, long-term use of certain drugs, and age, can induce a decrease in the mucus layer.
Symptoms:
PUD affects around 4.5 million Americans, for a prevalence of approximately 1.4 percent. Mild PUD symptoms include acid reflux, vomiting or nausea, bloating, and upper abdominal burning sensations. Heavy vomiting, occasionally blood-tinged, intense discomfort in the upper abdomen, tarry-black feces (indicative of a bleeding ulcer), and weight loss may occur in a severe case of peptic ulcer disease.Treatment:
Prescription medicines, in addition to a healthy diet, are required and can help treat the majority of peptic ulcers. Proton pump inhibitors, antibiotics, probiotics, or H2 receptor blockers may be administered depending on the underlying reason. However, in rare circumstances, the doctor may advise surgical excision of the ulcers.Crohn's Disease (IBD)
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Crohn's disease is an inflammatory digestive disease that can affect any portion of the gastrointestinal system, from the mouth to the anus. It is most usually associated with the ileum (the lower side of the small bowel) being ulcerated and inflamed. This ailment, like ulcerative colitis, is part of a category of gastrointestinal disorders known as inflammatory bowel disease (IBD).
Although the ileum is the most commonly affected by inflammation, ulceration can develop in any part of the small intestine, colon, esophagus, or stomach. Crohn's disease is most commonly diagnosed in people between the ages of 15 and 30, while it can occur at any age. According to the Crohn's & Colitis Foundation, about 780,000 people in the United States have Crohn's disease.
Symptoms:
Crohn's disease, like any other IBD, generally shows itself gradually, with certain symptoms worsening as the condition advances. Fever, weight loss, decreased appetite, exhaustion, bloody stools, stomach cramps, and diarrhea may occur in the early stages of the illness. Serious symptoms do not develop till much later. These can include ulcers, skin irritation, perianal fistulas, and anemia-related shortness of breath.Treatment:
Early screening and diagnosis can make a significant difference in your ability to begin treatment. Endoscopies (anesthesia-induced intubation of the upper and lower guts) and imaging examinations are used in the diagnosis procedure, which is overseen by gastroenterologists (X-rays, but also CT scans or Magnetic Resonance Enterography - MRE). Treatment options include:Medicine -
To reduce inflammation, you may need to take antidiarrheal medicines, anti-inflammatory meds, immunomodulators, antibiotics, and biologics.Dietary Modification -
Although no special dietary restrictions are normally required, a diet that has a modest influence on sections of the gut that might be constricted by inflammation is usually suggested. Your doctor and dietitian may also recommend additional, more complicated modifications.Surgical Procedure -
If lifestyle modifications and drugs do not work, this is a last-resort therapy option. However, three-quarters of Crohn's disease patients have elective surgery at some time.Ulcerative Colitis
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Along with Crohn's disease, ulcerative colitis is one of the two most prevalent inflammatory bowel illnesses (IBD). This diagnosis refers to a set of digestive illnesses that result in GI tract inflammation. Ulcerative colitis is caused by inflammation of the colon's (large intestine's) inner lining, the rectum, or both.
Symptoms:
Ulcers or tiny sores begin to form, usually in the rectum and extending to the large intestine. It is believed that over 750,000 people in the United States have ulcerative colitis, which is most commonly diagnosed in those aged 15 to 35. The presence of other immunological illnesses, as well as environmental factors such as antigens, viruses, and bacteria, may all enhance your chances of gettingulcerative colitis.
Diarrhea, frequently with bloodstains in the stool, fever, malnutrition, weight loss, stomach discomfort, and recurrent abdominal noises are the most prevalent signs of the illness. Other symptoms associated with UC include inflamed eyes, mouth sores, skin problems, loss of appetite, joint swelling, and joint discomfort.
Treatment:
Of course, proper diagnostic measures are required, which will most likely entail a colonoscopy and will be supervised by a gastroenterologist. The optimal course of therapy will be determined depending on the severity of the problem and other circumstances, and will commonly involve prescription medications such mesalamine, sulfasalazine, balsalazide, or olsalazine, as well as steroids to assist reduce swelling and inflammation.Antibiotics, probiotics, and other treatments that may help decrease immune activity, as well as biologic therapies that help block inflammation, may be prescribed by the doctor. The therapy is usually lengthy, and it may last a lifetime. Because the problem does not reach up to the small intestine, surgery to remove all or sections of the colon and rectum may be considered in tough instances.
Gallstones
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Gallstones are exactly what their name implies: stone-like masses that form in the bile ducts or gallbladder. They can range in size from a grain of sand to a golf ball. The gallbladder is a tiny digestive organ in the upper right belly. Its function is to create, store, and release bile, a yellowish-green fluid that assists in fat digestion. This is a rather prevalent disorder in the United States, affecting 10-15% of the general population. Although the precise reason is unknown, gallstones often occur when bile has a high proportion of bilirubin and cholesterol. Ultrasound is used to make the diagnosis, which is occasionally aided by endoscopy to detect tiny stones.
Symptoms:
Gallstones can cause no symptoms, but most patients suffer pain in the upper right abdomen, especially after eating fatty meals. Indigestion, diarrhea, burping, dark urine, vomiting, nausea, and clay-colored feces are also signs of gallstones. People who have minor or no symptoms may not require therapy.Treatment:
Depending on the symptoms, surgery to remove the gallstones may be necessary. Each year, around 250,000 Americans with gallstones have surgery. Bile is no longer stored in the gallbladder without the gallbladder, therefore it goes directly from the liver into the small intestine. This, however, has no effect on regular digestive function. If the gallstones are trapped in the bile ducts, endoscopy is typically recommended.Pancreatitis, both acute and chronic
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
Pancreatitis, or pancreatic inflammation, affects both adults and children. It is the most prevalent pancreatic condition, causing significant morbidity and occurring in either acute or chronic forms (death). Pancreatitis, once considered to be uncommon, has been growing for at least the past 20 years and is now thought to be comparable in adults and children, with up to 80 cases per 100,000 in the general population.
The prevalence is rising globally, owing mostly to rising rates of obesity and gallstones. The acute type of pancreatic inflammation, a J-shaped organ that secretes digesting enzymes and hormones, arises quickly and lasts for several days. Mild instances of acute pancreatitis normally resolve on their own, but severe cases can result in life-threatening consequences.
Chronic pancreatitis, on the other hand, is a less frequent kind of pancreatitis that lasts for months or years and is associated with potentially serious consequences such as pancreatic cancer. The following are the most common avoidable causes of pancreatitis in adults:
- Alcoholism
- Smoking cigarettes
- Obesity
- Injuries to the abdomen
Symptoms:
Symptoms usually appear abruptly and are characterized by stomach pain that can reach to the back, often feeling stabbing and made worse by eating, nausea, and vomiting. Acute pancreatitis can potentially lead to significant consequences such as pseudocysts (pockets of fluid in the pancreas that might burst), necrotizing pancreatitis (death of pancreatic cells), diabetes, and kidney failure.Treatment:
Chronic pancreatitis can also cause unintentional weight loss (which can lead to malnutrition) and greasy stools. The diagnosis is based on blood tests that assess pancreatic enzyme levels and is supplemented by imaging studies such as ultrasounds and/or CT scans. Specific genetic testing can also be used to determine rare hereditary variants of chronic pancreatitis (Hereditary pancreatitis).Fasting, IV fluid infusions, pain medication, and other interventions depending on the diagnosed reason must all be done in a hospital setting.
Liver Disease
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
While the causes vary, they can all harm your liver and impair its function. According to the CDC, 1.8 percent of US adults have chronic liver disease, which amounts to around 4.5 million Americans. A gastroenterologist or primary care physician can detect liver disease using blood testing, or through imaging studies such as CT or MRIs.
Symptoms:
Depending on the cause, the symptoms of liver disease might differ from person to person. Itchy skin, chronic exhaustion, vomiting, nausea, bloated belly, legs or ankles, dark urine, jaundice, loss of appetite, and black or bloody feces are some of the common symptoms.Treatment:
For liver illness, lifestyle adjustments are frequently advised. These may include limiting or eliminating alcohol consumption, which is a common cause of serious liver disease, maintaining a healthy weight (obesity is often associated with a chronic inflammation of the liver known as Non-Alcoholic Fatty Liver Disease), drinking plenty of water, and adopting a low-fat, "liver-friendly" diet.Depending on the underlying reason, the doctor may give antibiotics, blood pressure meds, steroids, antiviral treatments, and multivitamins. On rare circumstances, surgery to remove diseased sections of the liver may be required. If no other treatment options are available, a liver transplant may be required.
Diverticulitis
 |
| Most Common Gastrointestinal Symptoms and What to Do About Them |
The situation Diverticulosis is defined by the creation of tiny pockets or pouches termed diverticula in the bottom region of the colon's inner lining (the large intestine). Diverticulitis is the inflammation of these waste-filled spaces, which become infected. This can result in a variety of minor to severe consequences, including rectal bleeding. Diverticulitis is a complication of severe or advanced diverticulitis.
Symptoms:
Fevers and chills, nausea and vomiting, excruciating stomach cramps, bloody stools, and rectal bleeding may be the only symptoms or they may be more severe.Treatment:
Diverticulitis can be managed in a variety of ways, including:Dietary changes -
Your doctor may put you on a liquid-only diet for a few days before gradually introducing low-fiber meals.Medication -
You may be offered OTC pain relievers as well as antibiotics if you have an infection.Surgery -
This is a last resort if medicine and dietary modifications are ineffective in treating your diverticulitis. These may involve intestinal resection with colostomy or anastomosis, as well as needle drainage.Summary
The gastrointestinal tract is a huge organ system that performs multiple functions such as food digestion, vitamin and fluid absorption, protection from invading microorganisms or noxious chemicals, and waste elimination. Any ailment that affects the digestive system is classified as a gastrointestinal disorder. It is estimated that these illnesses impact 60-70 million individuals in the United States alone, resulting in a quarter-million fatalities per year.While symptoms vary according to the ailment and underlying cause, most gastrointestinal disorders have similar symptoms such as abdominal discomfort, diarrhea, constipation, bloating, weight loss, and excess gas.
To summarize, the most prevalent digestive problems are:
Celiac disease
Is an autoimmune digestive ailment in which the body's immune system reacts to gluten. While the actual etiology is unknown, genetics and environmental variables like as viral infections may play a role in celiac disease development.Irritable Bowel Syndrome (IBS)
Is a disorder that causes stomach discomfort or bloating as well as diarrhea or constipation (or both).Lactose intolerance -
This condition develops when a person is unable to digest lactose, a sugar present in milk and processed dairy products. This is due to a deficiency of lactase, an intestinal enzyme that typically digests lactose.Chronic diarrhea -
This is a condition in which a person has four or more weeks of watery or loose stools. This chronic diarrhea can be caused by a variety of factors, including dehydration and inadequate nutrition.Constipation -
Over 2.5 million people in the US suffer from this very common digestive ailment. A dry, stiff stool that makes it difficult to evacuate the intestines causes constipation.GERD (Gastroesophageal Reflux Disease) -
This condition is distinguished by frequent bouts of acid reflux from the stomach into the esophagus, which can gradually destroy the esophagus. A person suffering from GERD has heartburn and acid reflux symptoms at least twice a week.Peptic ulcer disease
Occurs when lesions grow on the lining of the gastrointestinal system. PUD symptoms include changes in appetite, vomiting, chest discomfort, indigestion, weight loss, and bloody feces.Crohn's disease
Is a chronic inflammatory bowel disease (IBD) characterized by inflammation of any region of the gastrointestinal system, most often the lower small and large intestines.Ulcerative colitis
Inflammatory bowel illness of another kind. In UC, open sores and inflammation damage the colon's lining. Additionally, this illness has a long history that involves fever, malnutrition, diarrhea, and bloody stools.Gallstones
These are tiny stone-like particles that develop in the bile-storing gallbladder when bilirubin and cholesterol levels are high. Gallstones can cause pain in the upper abdomen, burping, dark urine, nausea, and clay-like stools, among other symptoms.Pancreatitis, both acute and chronic
Inflammation of the pancreas, an organ responsible for the production of digestive fluids as well as hormones. Severe stomach discomfort, nausea, vomiting, and weight loss are common symptoms. While acute pancreatitis can be caused by a variety of reasons, including infections, alcohol is responsible for more than two-thirds of chronic pancreatitis occurrences.Disease of the liver -
This term encompasses all diseases, problems, and disorders affecting the liver, including liver cirrhosis. Pale stools, dark urine, jaundice (or yellowing of the eyes and skin), appetite loss, nausea, and vomiting are all common symptoms. Treatment options differ according on the underlying cause.Diverticulitis
When one or more diverticula (small pouches or pockets that develop on the GI lining as a result of diverticulosis) become inflamed and infected, this disease arises. While common symptoms such as constipation, diarrhea, and bloating are minor, advanced diverticulitis can result in rectal bleeding and other serious digestive issues.It is critical to contact a gastroenterologist if any of the symptoms of a diagnosis or treatment plan continue.



.jpg)

0 Comments